Heart failure is a severe and often progressive condition that occurs when the heart is unable to pump enough blood to meet the body’s needs. It can stem from various underlying causes, including coronary artery disease, high blood pressure and heart valve issues.
Dr. Michael Kwan, transplant cardiologist and program director for the Advanced Heart Failure and Cardiac Transplant Program at Methodist Hospital, the largest heart transplant program in South Texas, said there are many ways to manage and treat heart failure, including an array of therapies and, in some cases, life-saving solutions like heart transplants.
When is a heart transplant necessary?
The decision to move forward with a heart transplant is made when all other treatment options have been unsuccessful. In advanced heart failure, doctors carefully consider a patient’s condition and attempt a variety of medications and treatment before recommending a transplant.
According to Kwan, patients must meet specific criteria, including recurrent heart failure due to low cardiac function and failure to respond to standard medical therapies.
Currently, the four classes of medications -- beta blockers, RAAS inhibitors, mineralocorticoid antagonists and SGLT2 inhibitors -- are considered the standard of care for heart failure.
“Those four different medical therapies are now the standard of care. So, they must be on all four and still doing poorly,” Kwan said.
If the patient has failed all these treatments, that’s when doctors will consider cardiac replacement therapies like matricular assist devices or cardiac transplantation.
Doctors must do an extensive workup to determine the patient is a candidate for a transplant.
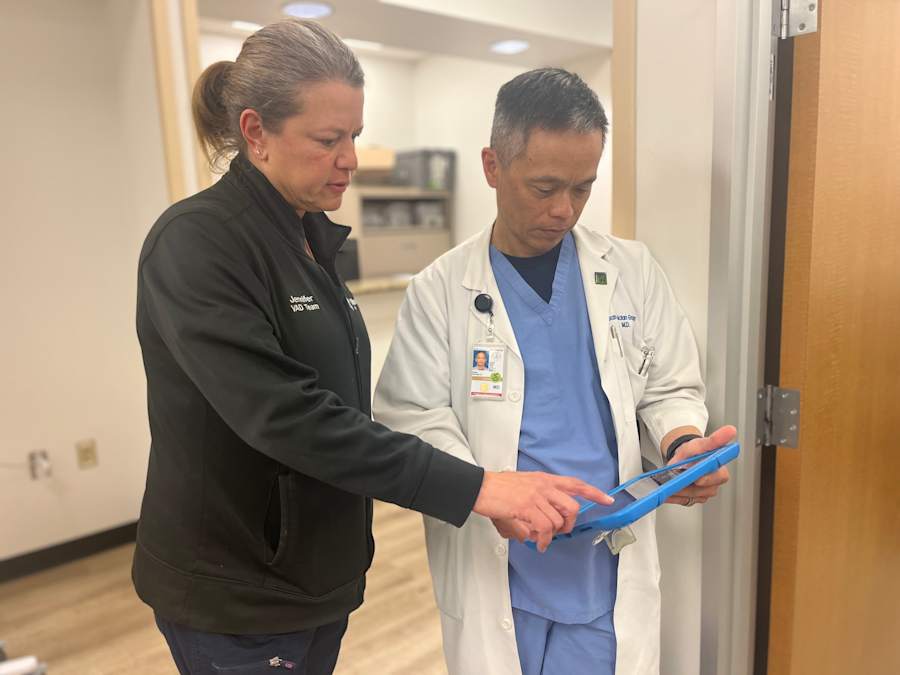
The role of multidisciplinary teams in heart transplant evaluation
Heart transplantation is a complex procedure. As a result, a multidisciplinary team approach is vital to evaluate whether a patient is a suitable candidate.
Transplantation affects not just the heart but also other organs, such as the kidneys, liver and endocrine system, due to the immunosuppressive medications required after surgery. This is why cardiologists, nephrologists, pulmonologists, gastroenterologists and other specialists work together to assess a patient’s overall health and the likelihood of success post-transplant.
“You need this multidisciplinary evaluation to make sure the other organs are up for it,” Kwan said.
During the evaluation, the goal is not just to ensure that the patient survives the surgery but that they can thrive long-term post-transplant, without complications arising from other conditions like cancer, stroke or kidney failure.
Alternatives to heart transplant: Mechanical devices and therapies
Patients who are not a candidate for a heart transplant aren’t left with no options. According to Kwan, patients who cannot tolerate anti-rejection medications may benefit from a mechanical device, such as a ventricular assist device (VAD). These devices can assist in pumping blood and may be used as a bridge to recovery or to support the heart until a transplant is possible.
“We can use these to try to get the patient out of the acute state that they’re in,” Kwan said.
In some cases, patients may also benefit from intravenous therapies aimed at supporting the heart. Additionally, temporary devices, like ECMO (extracorporeal membrane oxygenation), can support both the heart and lungs, allowing the heart to rest and recover. These options provide hope to patients who are not transplant candidates, offering a chance at improved quality of life or recovery.
“That’s one of the big advantages at Methodist Hospital,” Kwan said. “We can treat the full spectrum of disease and shoot for recovery, which is always the best possible solution.”
The heart transplant process: From waitlist to surgery
Once a patient is placed on the transplant list, the waiting period can vary based on factors like blood type, body size and the patient’s overall condition.
On average, patients may wait six to 12 months for a heart, though patients hospitalized with severe heart failure may only wait three to four months.
Kwan said the wait time is heavily influenced by regional factors and organ availability.
Once a suitable donor heart is found, a highly coordinated process begins. Surgeons at the recipient hospital must be prepared to act quickly, as the new heart must be implanted shortly after being harvested.
“We’ll have our patients come into the hospital, prep them for surgery and do labs to ensure there’s nothing else going on that would preclude a transplant, like an infection, for example.”
Doctors will take the recipient to the operating room, all while keeping close coordination with the donor hospital as Methodist Healthcare surgeons go to where the donor heart is to harvest it.
It’s an intricate dance between multiple parties, during which the recipient can be in the OR anywhere from six to eight hours, on average. Patients can expect to stay in the hospital for one to two weeks post-surgery.
Kwan said he strongly encourages people to have discussions with their loved ones the in event the unthinkable should happen. Make the decision now about whether you would want your organs donated, because it might have the potential to save someone’s life one day.
“These organs come from the generosity of people who have the foresight to think of something unforeseeable or catastrophic that could happen,” he said. “They take comfort in the fact that something good can come out of the worst day of their lives. I think that awareness is important.”
Recovery after a heart transplant
The recovery process following a heart transplant is extensive and requires both physical and emotional adjustments. Immediately after surgery, patients must focus on allowing their chest bones to heal while also learning how to manage their new medications.
“They must learn not to pull themselves up by their arms, not to push themselves up out of the bed, because they need their breastbone to heal. They also have to learn their new medications. We do quite a bit of teaching, not only to the patient, but to the family members, as well.”
Patients must adhere to strict schedules for taking medications like immunosuppressants and steroids, which help prevent rejection but also have significant side effects.
A patient’s discharge depends not just on their condition but on the teaching process, because the recipient and their family must learn a whole new lingo, as well as new signs and symptoms to look for.
In the first year post-transplant, patients will have frequent follow-up appointments to monitor for signs of rejection, adjust medication levels and ensure proper heart function.
“It’s a series of scheduled follow-ups: 12 within the first year, which are kind of front loaded. It’s weekly for the first month, biweekly for the next month, then monthly. We gradually space it out as they get further and further from the transplant date.”
Rejection is a possible complication after a heart transplant. Most cases of rejection respond to treatment, but in severe cases, retransplantation may be necessary. Kwan said majority of rejection cases are treatable and, with proper management, patients can continue to thrive.
A comprehensive approach to heart failure treatment
Kwan said the heart failure and transplant program at Methodist Hospital is unique because of its comprehensive approach. Beyond transplant services, the hospital offers a wide range of medical therapies and surgical options for heart failure patients.
The program’s strength lies in its ability to tailor treatments to each patient, offering not just transplant options but therapies that can improve heart function and prevent the need for a transplant.
“It’s one set of providers. It’s the same doctors who follow you throughout the course, so they know you start to finish.”
A wide range of specialists work together to manage all aspects of heart failure, ensuring that patients receive the most comprehensive treatment available. This collaborative approach is key to achieving excellent outcomes, including reduced rejection rates and better survival rates for transplant patients.
To learn more about the Methodist Heart Failure and Cardiac Transplant Program at Methodist Hospital, click or tap here.
For more than 60 years, Methodist Healthcare has delivered exceptional heart, lung and vascular care to all ages. As the largest heart care program in South Texas, Methodist Healthcare is home to a skilled team of cardiovascular specialists who expertly treat heart attacks, heart disease and cardiovascular disease, across eight hospitals and 40 clinics in Greater San Antonio.



